Nature Communications Publication: Reaching New VISTAs
Sensei recently announced the publication of a peer-reviewed research paper in Nature Communications entitled “VISTA checkpoint inhibition by pH-selective antibody SNS-101 with optimized safety and pharmacokinetic profiles enhances PD-1 response.”
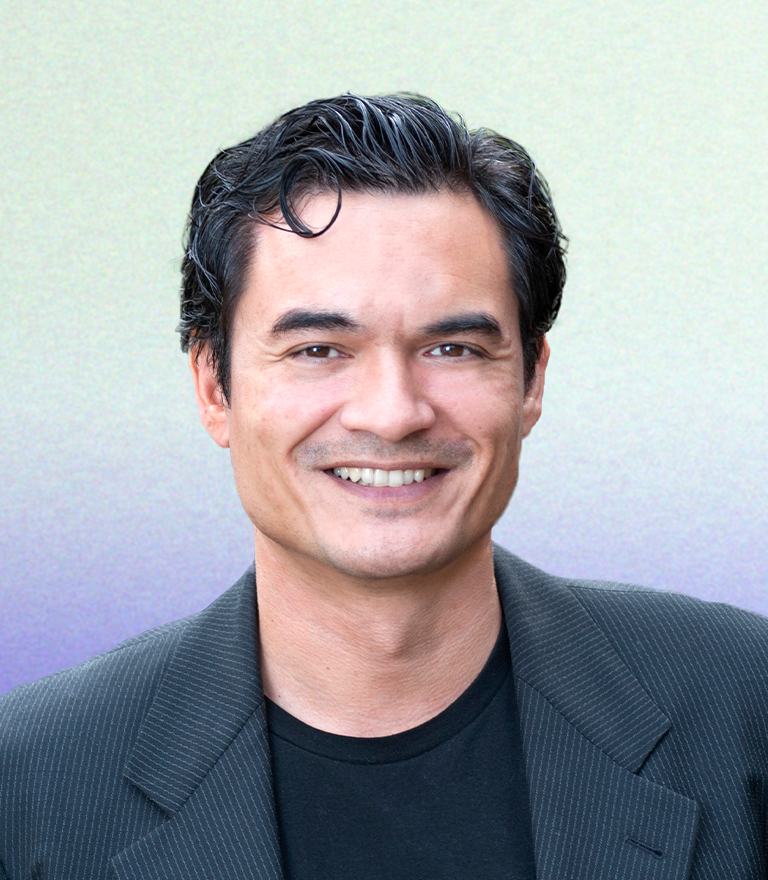
The paper describes Sensei Biotherapeutics’ approach to the discovery and development of SNS-101, which was designed to potently and selectively target the active protonated form of VISTA, a protein that plays a significant role in suppressing T-cell activation. The paper details the mechanism and characteristics of SNS-101, a novel pH-sensitive monoclonal antibody. SNS-101 was shown to bind to a novel epitope of VISTA that is remodeled under low pH conditions, switching VISTA into an active state that engenders extensive T-cell suppression. This Q&A with senior author, Edward van der Horst, Sensei’s Chief Scientific Officer, explores important takeaways from this publication.
Question: From your perspective, why is this publication important and what are key takeaways?
Edward:
We believe the publication of this research in Nature Communications, a high impact journal, serves as important validation for our tumor-targeting approach and confirms our ability to design a highly selective antibody that targets VISTA under the unique conditions of the tumor microenvironment.
When designing a highly selective antibody that targets VISTA, we now understand that it’s important to consider pH sensitivity and specificity. SNS-101 is designed to be pH-sensitive, which enables selective binding to its target, VISTA, at specific pH levels. This property is crucial for its action in the tumor microenvironment, which often has a lower pH compared to normal tissues. Additionally, the co-crystal structure of the antibody with VISTA has been elucidated, showing how the antibody binds to VISTA and blocks its interaction with key receptors, primarily PSGL-1.
It’s also important to note that blocking VISTA disrupts its role in immune regulation, notably modulating T cells toward an anti-tumor phenotype, potentially abrogating key checkpoint resistance mechanisms. Taken together, these actions address previous challenges with targeting VISTA, potentially offering a therapeutic strategy without inducing adverse effects like cytokine release syndrome (CRS).
Lastly, this paper provides mechanistic insights into the tumor microenvironment. SNS-101 also modulates the tumor microenvironment by altering the expression of specific cytokines and chemokines. It shifts the balance from an immune-suppressive, M2-like macrophage network to a pro-inflammatory, M1-like phenotype. This repolarization contributes to its anti-tumor effects.
Question: What makes the tumor microenvironment unique?
Edward:
Where to start? The tumor microenvironment (TME) is particularly inhospitable to T cells due to its acidic nature and the presence of immune-suppressive elements. This acidity, a defining characteristic of the TME, is detrimental to T cells, which are essential for mounting an effective immune response against cancer cells. In addition to the low pH, the TME is laden with soluble factors and cell populations that further suppress immune activity and contribute to hostile conditions.
Visualizing the tumor as a spherical mass, the TME can be likened to a surrounding halo that creates a barrier, not just physically but also functionally, against immune system penetration and activity.
The acidity of the TME is a result of the altered metabolic processes of tumor cells. Unlike normal cells, which primarily use glucose for energy, tumor cells predominantly use glucose as a building block for growth and proliferation. This metabolic shift leads to the production of acidic byproducts, thereby lowering the pH of the surrounding environment. The acidification of the TME is a direct consequence of the tumor’s metabolic demands and impedes the immune system’s ability to effectively target and eliminate the tumor.
Question: Why was VISTA previously considered undruggable? How has this research brought this important target within reach?
Edward:
The paper details the mechanism and characteristics of SNS-101, which is designed to block VISTA by inhibiting its interaction with PSGL-1 on T-cells resulting in T-cell activation. Subsequently, in various preclinical models, SNS-101 was shown to mitigate CRS risk and maintain a favorable pharmacokinetic and safety profile, all of which had thwarted the clinical development of first generation, non-pH sensitive anti-VISTA antibodies.
Addressing the challenge of selectively targeting VISTA-positive cells within the tumor microenvironment, while sparing similar cells in peripheral blood, is complex due to the ubiquitous presence of myeloid lineage cells, such as monocytes, macrophages, and neutrophils. These cells are abundant in both tumors and peripheral blood, with neutrophils being the most prevalent in circulation.
Previous attempts to target VISTA, like the clinical trial initiated by Johnson & Johnson (J&J) in 2016, faced setbacks. The trial was halted and eventually terminated after a patient developed severe CRS at a relatively low dose, highlighting the risks associated with targeting VISTA in a non-selective manner.
The innovation in this context is the development of a pH-sensitive antibody that discriminates between VISTA-positive cells in different environments. This antibody is designed to bind to VISTA only under acidic conditions, such as those found in the tumor microenvironment, where the pH is lower due to factors like hypoxia and metabolic activity. In contrast, in the neutral (physiological) pH of peripheral blood, the antibody does not bind to VISTA, avoiding the activation of immune responses that could lead to complications like CRS. This selective binding mechanism, activated only in the acidic conditions of the tumor site, represents a strategic approach to targeting VISTA while minimizing side effects induced in the periphery.
Question: What is target mediated drug disposition? Why is this a challenge for certain classes of drugs and, in particular, VISTA?
Edward:
The concept of target-mediated drug disposition refers to the phenomenon where an antibody, after binding to its target on the cell surface (such as VISTA), triggers the internalization of the antibody-target complex into the cell. This process results in the degradation of the antibody within the cell, while the target molecule is recycled back to the cell surface. This creates a continuous cycle of binding, internalization, degradation, and re-expression of the target.
In the context of VISTA, this mechanism poses a significant challenge for therapeutic antibody targeting because it leads to the rapid elimination of the antibody from the bloodstream. Consequently, the abundance of VISTA-positive cells, the internalization and degradation process make it difficult to maintain therapeutic levels of the antibody in the system.
This elimination process follows Michaelis-Menten kinetics, which is typical for enzymes but in this case applies to the interaction between the antibody and its target. The challenge is not specific to any particular antibody but is inherent to the biological process involving VISTA.
Question: Considering the challenges of past approaches, how did you go about defining the profile for a novel anti-VISTA antibody, SNS-101?
Edward:
The development of SNS-101 was guided by the critical need to avoid the adverse effects seen with previous therapies targeting myeloid cells, such as CRS and poor pharmacokinetic (PK) profiles. This led to two imperative design criteria.
- Strict pH-dependent binding. We knew the antibody had to exclusively bind to VISTA under acidic conditions, akin to the tumor microenvironment, and show no binding affinity in physiological pH. This stringent specificity is designed to minimize the risk of systemic side effects and ensure that the therapeutic action is localized to the tumor site. One might ask, what’s the pH of tumors and what’s the range? Tumor-like environments have been reported between 5.6 and 6.8. We have demonstrated a coverage range of 5.8 to 6.4—a very good portion of that reported acidic tumor microenvironment. Well, what if it is above—what if we encounter a pH seven, for example? Well, in that case, VISTA is not protonated, meaning the antibody will not bind. But importantly, VISTA is not active and therefore cannot interact with its counterreceptor on T cells.
- Comprehensive evaluation for safety and efficacy. Extensive preclinical research was undertaken to ascertain that SNS-101 would not trigger CRS. This included a range of studies from in vitro experiments with human whole blood to in vivo testing in a humanized mouse model specifically engineered for evaluating cytokine release. Further, toxicology studies in non-human primates were conducted to affirm the safety profile of the antibody.
Question: Tell us about some of the most challenging experiments one has to perform for a pH-sensitive approach? What makes this approach more technically challenging than a traditional antibody approach?
Edward:
The challenge in testing the pH-sensitive antibody arises from its unique binding property, which only occurs at low pH levels, conditions under which classical in vitro experiments are not typically conducted. This specificity necessitates modifying standard experimental conditions to mimic the acidic tumor microenvironment where the antibody is active, creating a challenge since T cells, crucial for immune response, struggle to survive in such acidic conditions. To address this, extensive experimentation was required, particularly focusing on CRS assays. Unlike typical studies where one or two assays might suffice to assess the risk of CRS, the unique nature of this antibody led to the execution of four to five different assay systems to robustly confirm that the antibody does not trigger CRS. This was critical to ensure the safety and viability of the therapeutic program. The research involved not only adapting in vitro assays to function at lower pH levels but also developing specialized in vivo models in collaboration with partners. This comprehensive approach was necessary to thoroughly evaluate the antibody’s behavior and safety profile in conditions that accurately reflect its intended operational environment within the human body.
Question: What were some of the key discoveries or technological advances that enabled Sensei’s innovative approach?
Edward:
The strategic approach to developing an effective therapy against tumors hinges on three critical factors:
- pH Selectivity: The therapy must be selectively active in the acidic conditions of the tumor microenvironment. This selectivity ensures that the therapeutic agent, such as an antibody, targets and affects the tumor cells while minimizing impact on healthy tissues, which exist in a more neutral pH environment.
- Targeting Specific Interactions: It is crucial to inhibit the interaction between VISTA and PSGL-1. The rationale for focusing on PSGL-1, among other potential receptors, is its dual role as a checkpoint inhibitor. Not only is PSGL-1 involved in regulating CD4 T cell functions, but recent discoveries also highlight its role in the exhaustion of CD8 T cells. This makes PSGL-1 a significant target for reversing immune suppression and reactivating the immune system’s ability to combat tumor cells.
- Appropriate Fc Region (IgG1): The choice of the Fc region, specifically IgG1, is pivotal. This region of the antibody determines its interactions with immune effector cells and is crucial for eliciting an appropriate immune response. The IgG1 Fc region is known for its ability to engage with immune cells and mediate effector functions, which are essential for the therapeutic efficacy of the antibody.
These three key elements—pH-selective binding, targeted inhibition of the VISTA-PSGL-1 interaction, and the utilization of an IgG1 Fc region—combine to form a targeted therapeutic approach that aims to effectively modulate the immune response within the tumor microenvironment, countering the tumor’s immune-suppressive tactics and stimulating an effective anti-tumor immune response.
Question: How does this research build on and further validate Sensei’s tumor-targeting approach?
Edward:
The development of pH-sensitive antibodies is a strategic approach that allows for selective targeting of the tumor microenvironment, as evidenced by various programs like SNS-201, which utilizes a dual-targeting approach: one arm of the antibody is pH-sensitive and targets VISTA, serving primarily as a targeting mechanism within the acidic tumor microenvironment. The other arm of the antibody targets CD28, an immune costimulatory receptor, and functions as an agonist to activate T cells. This bifunctional approach leverages the acidic conditions of the tumor microenvironment to localize and enhance the therapeutic action, ensuring that VISTA targeting is utilized not just for blocking interactions but also as a means to direct the antibody to the tumor site. The CD28 agonistic portion then actively engages the immune system, specifically T cells, to promote an anti-tumor response. This method showcases an innovative way of using the tumor’s acidity and the antibody’s dual functionalities to achieve targeted and effective immunotherapy.
Question: What are the broader implications of this research for the IO therapeutic landscape?
Edward:
The significance of targeting VISTA in cancer therapy lies in its potential role in overcoming resistance to checkpoint inhibitors. Although VISTA has not been clinically validated as a checkpoint target, both genetic and pharmacological evidence suggest that combining VISTA and PD-1 blockade can synergistically enhance anti-tumor responses.
VISTA might act as a compensatory checkpoint that becomes more dominant following the failure of other checkpoint therapies like PD-1 inhibitors. Therefore, targeting VISTA with SNS-101 could potentially enhance or restore the efficacy of PD-1 blockade, addressing both primary resistance (where patients do not initially respond to treatment) and adaptive resistance (where patients develop resistance after initial response). Where PD-1 inhibitors show minimal efficacy, VISTA targeting could potentially provide a new therapeutic avenue.
Ultimately, the goal with SNS-101 and similar molecules is to increase the proportion of patients who benefit from checkpoint therapy, extending and enhancing the durability of their response. By integrating VISTA targeting into the treatment regimen, especially in combination with PD-1 inhibitors, we believe there is potential to improve outcomes for patients who have previously failed checkpoint therapy, broadening the scope of effective cancer immunotherapy.
+++
This research was conducted by scientists at Sensei Biotherapeutics in collaboration genOway and with the laboratory of Dr. Robert Schreiber at the Washington University, St. Louis School of Medicine. The manuscript published in Nature Communications can be found here: https://rdcu.be/dDF8x
Cautionary Note Regarding Forward-Looking Statements
Any statements contained in this article that do not describe historical facts may constitute forward-looking statements as that term is defined in the Private Securities Litigation Reform Act of 1995. These statements may be identified by words and phrases such as “believe”, “designed to,” “expect”, “may”, “plan”, “potential”, “will”, and similar expressions, and are based on Sensei’s current beliefs and expectations. These forward-looking statements include expectations regarding the development of Sensei’s product candidates and platforms, including SNS-101; the potential safety profile of Sensei’s product candidates, including SNS-101; and the potential benefits of Sensei’s product candidates, including SNS-101. These statements involve risks and uncertainties that could cause actual results to differ materially from those reflected in such statements. Risks and uncertainties that may cause actual results to differ materially include uncertainties inherent in the development of therapeutic product candidates, such as the risk that any one or more of Sensei’s product candidates will not be successfully developed or commercialized; the risk of delay or cessation of any planned clinical trials of Sensei’s product candidates; the risk that prior results, such as signals of safety, activity or durability of effect, observed from preclinical studies will not be replicated or will not continue in ongoing or future studies or clinical trials involving Sensei’s product candidates; the risk that Sensei’s product candidates or procedures in connection with the administration thereof will not have the safety or efficacy profile that we anticipate; risks associated with Sensei’s dependence on third-party suppliers and manufacturers, including sole source suppliers, over which Sensei may not always have full control; risks regarding the accuracy of Sensei’s estimates of expenses, capital requirements and needs for additional financing; and other risks and uncertainties that are described in Sensei’s Annual Report on Form 10-K filed with the U.S. Securities and Exchange Commission (SEC) on February 29, 2024 and Sensei’s other Periodic Reports filed with the SEC. Any forward-looking statements speak only as of the date of this content, and are based on information available to Sensei as of the date of this content, and Sensei assumes no obligation to, and does not intend to, update any forward-looking statements, whether as a result of new information, future events or otherwise.